For 10 years now, Christine Porciuncula, an entrepreneur from Valenzuela City, has been battling end-stage renal disease. While she says the mental stress stemming from her condition is challenging enough, getting by with her erratic income is another story.
Much of her budget is used to cover medical expenses. Money easily goes down the drain with her twice-a-week dialysis on top of the regular medical checkups and other medications.
With costs piling up, Porciuncula says she seeks the help of the Philippine Charity Sweepstakes Office (PCSO) and the local government of Valenzuela. More often than not, she would find herself in a long queue of aid seekers patiently waiting to be called. Such is commonplace in the Philippines, where more than half of the total health spending comes from a household’s out-of-pocket payments (OOP) based on the 2017 Philippine National Health Accounts.
A trip to the hospital always comes with costs. Based on the 2017 National Demographic and Health Survey, the average cost of treatment for confined individuals is PHP21,400. State-run Philippine Health Insurance Corporation or PhilHealth shoulders only less than half of this. This does not include the cost of medicines or services from external pharmacies and laboratories that amounts to an average of PhP5,237.
But with the recent signing of the Universal Health Care (UHC) Law in February, Porciuncula is among those pinning their hopes on its effective implementation.
“Hopefully, with this, I no longer have to fall in line to ask for financial help and worry where to get the money for my treatment,” Porciuncula said in an interview.
The landmark law expands access to health services by automatically enrolling all Filipinos in PhilHealth’s National Health Insurance Program (NHIP). It seeks to ensure that all Filipino citizens have access to a comprehensive set of health services without financial hardship.
Big Leap
For the National Economic and Development Authority, which led the crafting of the Philippine Development Plan (PDP) 2017-2022, the signing of the law is a big leap towards reforming the country’s health care system.
“Our medium-term plan recognizes human development not just as a means to economic development but as an end in itself. That is why the signing of the UHC law is a victory scored for the health sector. We are glad that we have reached this milestone halfway into the term of the Duterte administration,” Socioeconomic Planning Secretary Ernesto M. Pernia said.
The law aims to address a number of recurring problems in the health system. First and foremost, it assures 100 percent population coverage of PhilHealth—from the 98 percent population coverage in 2018 based on the same year’s Socioeconomic Report by NEDA.
According to the law, PhilHealth members will be classified into two groups: contributory (premium contributors from payroll) and non-contributory (fully subsidized from tax collections).
The law also addresses the fragmented and overlapping roles and responsibilities of various health agencies. For people like Porciuncula, this means that they will no longer have to hop from one charitable institution to another. For instance, the Department of Health (DOH) and local government units (LGU) will be responsible for population-based interventions and health services (e.g., immunization programs and health promotion programs) while PhilHealth will be responsible for financing individual-based health services.

In addition, the new law is expected to significantly reduce the high OOP expenditure for health. In 2017, about 54.5 percent of total health payment came from Filipinos’ own pocket, with medicines and drugs as the main contributors. Lack of Philhealth coverage of medicines for outpatients and the high cost of drugs and medicines in the country push the OOP expenditure up.
“High out-of-pocket medical expenses push more people into poverty. When households spend more on hospital bills and medical treatments, they are forced to spend less on other basic necessities like food, housing, and education,” Pernia said.
The accompanying results matrix of the PDP 2017-2022 targets out-of-pocket-medical expenses to go down to less than 50 percent of the total health spending by 2022.
Funding
According to the DOH, the implementation of the UHC law for its first year needs P257 billion. This will be sourced from sin tax collections and partly from income generated by the Philippine Amusement and Gaming Corporation (PAGCOR) and PCSO in view of improving benefit packages. This is apart from providing immediate eligibility and access to health services, including preventive, promotive, curative, rehabilitative, and palliative care, as well as out-patient drugs.
Pernia said the successful implementation of the sin tax reform law has been a boost to programs and projects of the DOH. Based on the agency’s budget brochures, DOH’s budget, including its attached agencies and corporations, increased by 13 percent from PHP151 billion in 2017 to PHP171 billion in 2018. This was due to PHP113-billion six tax revenues, of which PHP48 billion was allocated to PhilHealth’s premium subsidy for the indigent, senior citizens, and sponsored members.
The law also provides for a special health fund that will be created and managed by province-wide or city-wide health systems. All resources intended for health services will be pooled to finance population-based and individual-based health services. Such will also be used to cover operating costs, capital investments, and remuneration and incentives for all health workers.
The Department of Health, in consultation with the Department of Budget and Management and the local government units, is mandated to come up with guidelines for the use of the special health fund.
All income from Philhealth payments will go to the special health fund, which will be allocated by LGUs exclusively for the improvement of local health systems.
The crafting of the implementing rules and regulations, which will operationalize provisions in the law, such as budget allocations, health financing, improvements in the benefit packages, among others, is still ongoing. The law provides for a transition period (i.e., Section 41) for LGUs and concerned government agencies for the full implementation of the law.
Shortage
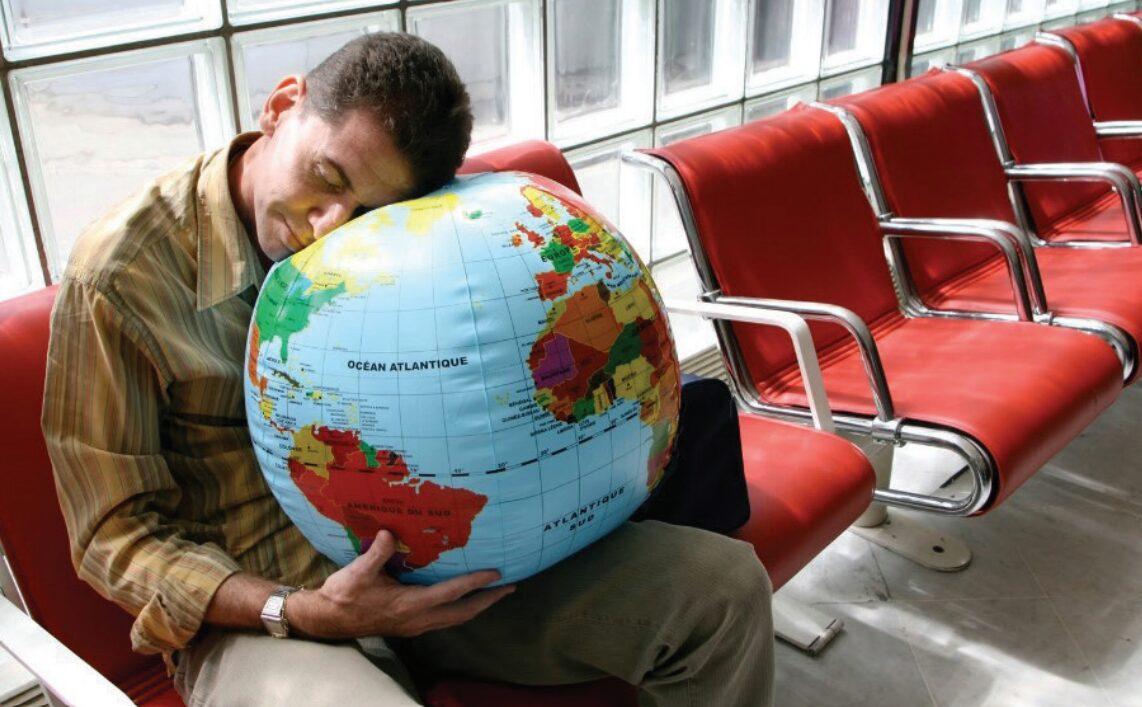
A 29-year-old nurse, Aira Cezar says, “We work for at least eight hours per day, but some of us extend for another eight hours if there’s understaffing within the unit. We always experience understaffing due to the exodus of nurses working abroad for better pay.” Cezar has been working for six years in a public hospital’s emergency room in Aklan.
The poor state of the population of health professionals in the country is another concern the UHC law intends to address. With the Philippines being a major exporter of health-care professionals, it constantly grapples with a shortage of health providers, inevitably leading to poor quality of healthcare and high-stress levels among health professionals.
The number of health workers in the country is not keeping up with the country’s population growth. According to the DOH, the nationwide ratio of human resource for health, which includes doctors, nurses, and midwives, is at 19.70 per 10,000 population. This is still below the 23 per 10,000 population critical threshold recommended by the World Health Organization (WHO).
Member countries of WHO, however, may opt to follow or not such recommendations. The Philippines’ DOH, for example, follows ratios published in the National Objectives for Health 2017-2022.[1]
The country also suffers from a disparity in the distribution of health workers in the country. For 2018, the National Capital Region and the Cordillera Administrative Region had the most number of health workers at 23.06 and 28.17 per 10,000 population while the Autonomous Region of Muslim Mindanao is a stark contrast at 6.86 per 10,000 population, according to DOH records.
For this reason, the UHC law ensures the development of the health system’s human resources through the formulation and implementation of the National Health Human Resource Master Plan. It also ensures that all health professionals have permanent employment and competitive salaries.
Similarly, the law provides for the creation of a national health workforce support system that will help local public health systems in addressing human resource needs while prioritizing deployment in the Geographically Isolated and Disadvantaged Areas (GIDAs).
“I have nothing against the UHC law. The idea is good as every Filipino will receive affordable and quality health benefits. But the law is useless unless the government starts to recognize the value of those working in the clinical sector,” Cezar said.
The law also tasks the Commission on Higher Education (CHED), Technical Education and Skills Development Authority (TESDA), Professional Regulation Commission (PRC) and the DOH to develop existing and new allied and health-related degrees and training programs, and to regulate the number of its enrollees depending on the needs of the population. The law provides scholarship grants for graduate and undergraduate allied and health-related programs.
All professional health graduates of government-funded scholarships will be required by law to render at least three years of return service with compensation under the supervision of the DOH. Incentives will be given to those who will render an additional two years of return service.
More Reforms
Secretary Pernia said more reforms should be done to ensure the smooth implementation of the UHC law.
While the law already provides the mechanisms to improve health care in the Philippines, he said that actual rollout by all those concerned is crucial, starting with agency budgets.
“The DOH, for one, must efficiently utilize its budget to develop and strengthen health infrastructure and human resources,” Pernia said noting that the agency’s budget utilization rate was only 88 percent in 2017, according to the 2018 budget brochure of DOH.
Also, the NEDA official said the function of LGUs to provide health services, which was devolved through the Local Government Code of 1991, has not reflected in their health spending. The health spending of LGUs comprised only 20 percent of overall government spending on health in 2017, according to the Philippine Statistics Authority.
“The enactment of the UHC law is a defining moment for the Philippine health system. We, at NEDA, are optimistic that its implementation will open the doors for more reforms that will improve the health of Filipino people,” Pernia said.
He noted that the law brings the country closer to its collective long-term vision, AmBisyon Natin 2040, where all Filipinos live long and healthy lives and where healthcare is affordable and accessible.
[1] One medical doctor per 20,000 population; 1 nurse per 10,000 population; and 1 midwife per 5,000 population. Data from DOH show that 28% of provinces have attained the 1 MD/20,000 population, 99% have reached the 1 N/10,000 population, and 79% have achieved the 1 MW/5000 population.
—
Stay updated with news and information from the National Economic Development Authority by visiting their website at http://www.neda.gov.ph.